[00:00:00] Welcome friends, to the Heart Rate Variability Podcast. This week in Heart Rate Variability Edition, each week we explore the latest research and news in hrv, trauma recovery and biofeedback. Before we begin, a quick and important note. The information shared in this podcast is for educational and informational purposes only. It is not medical advice and it is not a substitute for working with a qualified healthcare professional. Please consult your own clinician before making any changes to medical or mental health care. I'm glad you're here for episode 24, because this week's collection of studies gives us a rare opportunity to zoom out and and then back in again. We're going to move from trauma and felt safety into theory building around autonomic dysregulation, then into prediction and monitoring using HRV in migraine and heart failure, and finally down to the molecular and neural level of how the vagus nerve senses blood volume itself. These papers are very different on the surface, but they tell a surprisingly coherent story about the nervous system safety and physiological intelligence. We'll begin with a clinical research article in the European Journal of Psychotramatology titled From Somatic Experiencing to Felt Safety Assessing the Effects of a Body Oriented Intervention in Adults with Various Degrees of Child Maltreatment by Jurgen Limavara, Billy Janssen, Jens Bernardson, Marilyn Cloyer and Monique C. Faltz. This paper is important for anyone working at the intersection of trauma and physiology because it directly tests something clinicians talk about all the time, but that has been hard to measure empirically. The experience of felt safety. The authors start from a well established problem. Adults with histories of child maltreatment often report a chronic lack of psychological safety and a disrupted sense of body boundaries. These experiences don't just live in narrative memory they show up as difficulties with social connection, effect regulation and embodied self awareness. Despite that, we still have surprisingly few evidence based interventions that specifically target felt safety at the bodily level. In this paper, the authors conducted two randomized experiments using a brief 60 minute body oriented intervention derived from somatic experiencing. In Study 1, they focused on adults who reported low psychological safety. 89 participants were randomized either to the somatic experiencing based intervention or or to a psychoeducation control condition. In study two, they focused on disrupted body boundaries with 55 participants again randomized to somatic experiencing or psychoeducation. The results are striking. In the first study, participants in the somatic experiencing group showed a large increase in psychological safety compared with controls with an effect size approaching 1. They also showed improvements in positive affect, reductions in negative affect and increased social connectedness. Importantly for this podcast, heart rate decreased and heart rate variability increased across groups, suggesting a shift toward greater parasympathetic regulation during the session. In the second study, participants receiving the somatic experiencing intervention showed a significant reduction in disrupted body boundaries and an increase in interoceptive awareness, which the authors propose as a key mechanism of action. What matters here is not just that HRV changed, but that changes in subjective safety, embodiment and physiology move together in a short time frame. This paper gives empirical support to something many clinicians sense intuitively felt safety is not just a cognitive belief, it is an embodied state that can be shifted through bottom up interventions. Even briefly. An HRV appears once again as a useful window into those state changes, not as a diagnostic label, but as a dynamic marker of autonomic context.
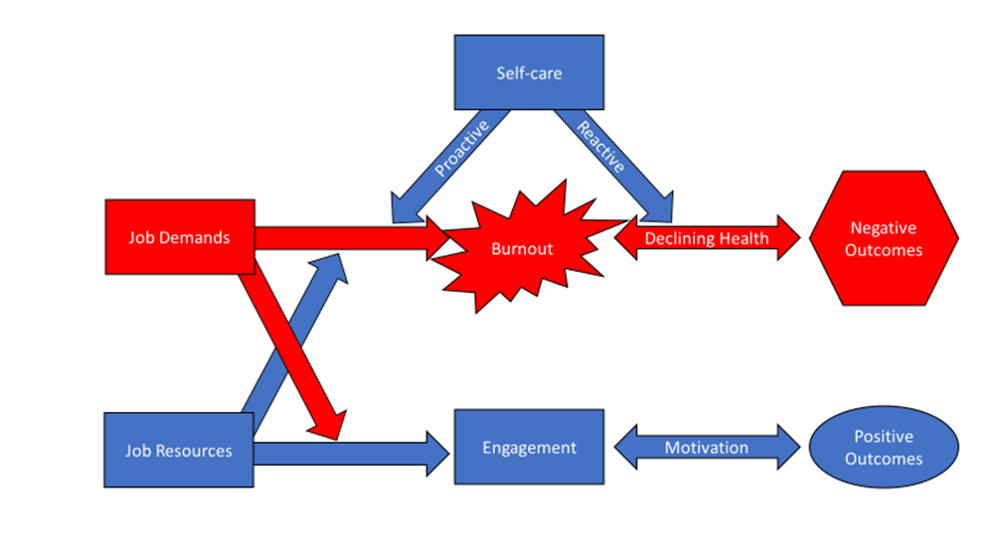
[00:03:08] From there, let's move into a very different kind of paper published in Frontiers in Psychology. This Hypothesis and Theory article titled Integrating Autonomic and Effective Pathways in Borderline Personality Disorder the Triangle Therapy Hypothesis was authored by Daniel Jurassic. This article is not an outcome study, it's a conceptual paper, and it's important to approach it that way. Jurazic starts from a critique that many trauma informed clinicians will recognize. While treatments like dialectical behavior therapy, schema therapy, and mentalization based therapy are effective for many people with borderline personality Disorder, they often work primarily at the cognitive and relational level. They may not directly engage the subcortical effect of an autonomic system shaped by early attachment trauma.
[00:03:45] Triangle therapy proposes a somatic pre phase intervention rather than a replacement for existing treatments. The model centers on three ancestral effective silence, sound, and isolation. These conditions are hypothesized to map onto early autonomic experiences related to neglect, abandonment, and overwhelming affect. The proposed protocol involves 30 sessions with progressive exposure to each condition under continuous therapist attunement, and without verbal interpretation. What's especially relevant for HRV clinicians is that this model explicitly frames therapy as autonomic integration or rather than symptom management.
[00:04:16] Jurassic hypothesizes that carefully titrated exposure to these effective conditions could recalibrate vagal and sympathetic tone, reduce catastrophic prediction errors, and allow symbolic processing to emerge later in treatment. HRV is not positioned here as a treatment target per se, but rather as a physiological readout to assess whether autonomic integration is occurring. This paper doesn't yet provide data, but it does offer language. It invites researchers to design studies that measure autonomic change not just as an outcome but as a mechanism and and it reminds clinicians that not all nervous systems can engage meaningfully in top down work until bottom up tolerance is established. Before we move on to the next set of studies, I want to take a moment to thank the sponsor of this episode. This week's episode of this Week in HRV is brought to you by Optimal hrv. At Optimal hrv, our mission is to make trauma informed evidence based biofeedback accessible to clinicians, researchers and individuals alike. Whether you're using HRV biofeedback in clinical practice, training students, or supporting your own nervous system regulation, Optimal HRV offers tools designed with both science and safety in.
[00:05:15] You can learn more about our app, clinician dashboards and education
[email protected] we're grateful for your support and for being part of this growing community. Let's now shift to prediction and monitoring, starting with a research article published online in Technology and Healthcare. The paper is titled Heart Rate Variability as a Predictor of Sleep Time Data Analysis of Pre Migraine Nights. Authored by Rudajenkovichut Viraslava Kapustynska and Vitaudis Abramovicius, this study tackles a question many migraine sufferers care deeply can we detect an impending migraine before symptoms fully emerge? The authors recruited 23 individuals with migraine and analyzed nocturnal HRV using wearable biosensors. They focused specifically on sleep time data, extracting HRV features from blood volume pulse signals and applying machine learning techniques to identify patterns preceding migraine attacks. What they found is not a simple universal signature, and that's actually the most honest and useful result. There was substantial individual variability in HRV responses during pre migraine nights. Some participants showed clear autonomic shifts, while others did not follow the same pattern. Rather than presenting HRV as a one size fits all predictor, the authors emphasize personalization. HRV may be useful for migraine prediction, but only when models are tuned to the individual's physiology. This approach aligns closely with what many of us see in practice. HRV is not a crystal ball, it's a context signal. When used longitudinally and individually, it may provide an early warning system that enables earlier intervention and reduced severity.
[00:06:40] This paper doesn't yet claim clinical readiness, but it lays important groundwork for personalized physiology driven migraine management.
[00:06:46] Staying with long duration monitoring. Let's move to a study published in Koreas titled Physiological Characterization of Severe Heart Failure Using Long Duration Ambulatory ecg A Retrospective Exploratory Analysis. The authors of this paper are Junaid Amir Khan, Usman Ali Mutanzi, Mahsan Ratan Chandra Roy Opmes Alamu, and Francesco Alessi Longa. This study uses approximately 20 hours of continuous ambulatory ECG data from 15 patients with severe heart failure classified as New York heart Association Class 3 or 4. Using the publicly available Beth Israel Deaconess Medical Center Congestive Heart Failure Database, the authors extracted heart rate, time and frequency domain hrv, and ECG derived respiration. What stands out here is the emphasis on heterogeneity and temporal dynamics across subjects. HRV was generally depressed, consistent with advanced autonomic dysfunction, but within subjects there was substantial variability over time. Heart rate and HRV did not always move in tandem. Underscoring the limitations of relying on a single metric. Early versus late segments of recordings often showed meaningful differences, suggesting residual circadian or arrest activity effects even in severe disease. This paper is explicitly exploratory it does not predict outcomes. Heart failure is not static, and neither is autonomic regulation. Hrv, especially when combined with respiratory proxies, offers a richer picture of physiological instability than episodic clinic visits ever could.
[00:08:07] Finally, we come to a paper that takes us all the way down to the neural sensors themselves.
[00:08:11] Published in Nature, this article is titled Vagal Blood Volume Compensate for Hemorrhage and Posture Change. The authors are Zhi Kai Liu, Sean Liu, Isabella A. Haskell, Michael S. Shop, Masha Josipovich, Su Hong Min, Abdul Rashid A. Alabi, Jinny Chee Min Seon Kim, and Stephen D. Liberus. This article is a landmark basic science paper, and although conducted in mice, its implications for HRV and autonomic science are profound. The authors identify a specific population of vagal sensory neurons that express the MechanoSensitive ion channel piezo 2. These neurons fire with every heartbeat and encode information about central blood volume, not just blood pressure. Using genetic knockouts, electrophysiology, calcium imaging, and optogenetics, the researchers show that these vagal piezo 2 neurons are essential for compensating for changes in posture and blood loss. When they are absent, animals develop orthostatic hypotension and fail to maintain blood pressure during hemorrhage, even when traditional baroreceptors are intact. For HRV researchers and clinicians, what matters is that this work clarifies something we often gloss over. The vagus nerve is not just a timing cable it is a rich sensory system that continuously reports mechanical information about the heart and circulation to the brain. Autonomic regulation depends on these sensory inputs. HRV in this context reflects not only central regulation but the integrity of peripheral sensing as we wrap up this week. I want to slow this down and make the takeaways explicit because this week's studies offer different lessons depending on who's listening. For individuals, the biggest message is that your nervous system is not broken, lazy or unpredictable. It is adaptive. The Somatic Experiencing study shows that even brief body oriented experiences can shift felt safety and autonomic state. That means regulation is not something you earn through discipline or force. It often emerges when the body is given conditions of gentleness, curiosity and choice. The migraine study reinforces this idea from another angle. Your physiology has patterns, but those patterns are personal. HRV is most useful when it helps you learn your rhythms, especially during sleep, rather than comparing yourself to norms. And the heart failure work reminds us that variability over time matters more than any single reading. Your nervous system tells a story across hours and days, not moments. For researchers, this week's papers collectively argue for moving beyond static models. The triangle therapy hypothesis proposed by Daniel Jureyshdeck invites experimental designs that treat autonomic regulation as a prerequisite for cognitive and relational work rather than merely an outcome. The migraine and heart failure studies underscore the importance of longitudinal within subject analyses rather than cross sectional averages. And the Nature paper reminds us that autonomic metrics like HRV are inseparable from sensory biology. Vagal tone reflects sensing as much as control. Future HRV research will be strongest when it integrates behavior, interoception, context and physiology into a single, coherent framework rather than treating HRV as an isolated signal. Taken together, this week's research points us toward a more mature understanding of hrv, not as a score to optimize, but as a language the nervous system uses to communicate safety, threat, capacity and recovery. When we listen carefully, whether as individuals, clinicians or researchers, that language becomes an ally rather than a verdict. Thank you for spending this time with me on the Heart Rate Variability podcast. If you found this episode helpful, please subscribe, share it with a colleague, or leave a review. Each week we'll continue exploring how physiology, psychology and healing come together through the lens of hrv. I'll see you next time.