[00:00:00] Speaker A: Welcome to the Heart Rate Variability Podcast. Each week we talk about heart rate variability and how it can be used to improve your overall health and wellness.
Please consider the information in this podcast for your informational use and not medical advice. Please see your medical provider to apply any of the strategies outlined in this episode. Heart Rate Variability Podcast is a production of Optimal LLC and Optimal HRV. Check us out at optimalhrv.com Please enjoy the show.
Welcome friends to the Heart Rate Variability Podcast. I am so excited for my guest today. She brings in two areas of expertise and work that I cannot wait to explore how she brings them together with occupational therapy and biofeedback. So I know if our listeners might not be as familiar with occupational therapy. Stay tuned. It's not just about something to do with a job. It can be, but it's so much more than that and I'm a huge fan of OT and obviously as listeners know a huge nerd around biofeedback. So Louise has given me the out not to try to pronounce her last name. So Louise, thank you for that Grace and I'd love just to allow you to say your name so our listeners have it and just a little bit of introduction on yourself and your work.
[00:01:32] Speaker B: Thank you Matt. Thanks for the opportunity. So yeah, my name is quite a long one, so it's Louise Van der Westhazen. So it's a. Yeah, quite a long surname. So fully understand. And I'm all the way from Cape Town in South Africa. So that's southernmost tip of Africa. Yeah, beautiful part of. Of the world.
[00:01:54] Speaker A: So I think you're our first guest from the continent of Africa. So yeah, I think we're ch off the list of continents and I believe you're the first one, so I'm excited to have you.
[00:02:11] Speaker B: Wonderful.
[00:02:12] Speaker A: Awesome. So for listeners who may not be as familiar with occupational therapy, I would love to just what does your tell me tell our listeners what occupational therapy is and a little bit about what that work looks like for you as an OT.
[00:02:33] Speaker B: Yeah, so I think OTs are trained, you know, and our main sort of focus is to look at functioning and functioning at various stages of development in life. So it can be your focus can be function and development, neurodevelopment in younger children if their sensory systems are well integrated or they're neural pathway development, whether that is optimized or not. So that's almost a field very much on its own, a super specialized field that we often called sensory integration or neurodevelopmental OTs.
And then you know, you can actually take occupational therapy through any domain of life. So it's whether there's a physical ailment or injury that needs rehabilitation post, say, accident, losing a limb or a stroke.
So we OT is really coming to place to say where did functioning have sort of. Yeah. Developed a difficulty and how can we retrain? So if we think about retraining, it can mean anything. So it's whether it's upper limb, lower limb, body, emotional as well. So my field really, where I come from is more in the field of mental health. So after my degree, I worked in the field of psychiatry most of the time. And then also places of safety, you know, where traumatized children removed from family. So you can get the feel how diverse it actually can be.
[00:04:15] Speaker A: Yeah, I love that. Can you go into. I would love. The sensory integration piece was just such a learning. I still to this day, it's been. I ran a school for special education children. That's where I got familiar with occupational therapists. If I probably got a little bit earlier, I might have a degree in it is how much I loved it. But I was just. And these were pretty extreme cases. A lot of nonverbal youth in their teenage years. So. But I was just. Just blown away how a bouncy chair or something I still use to this day, which is a weighted blanket, because I also have a sensory nervous system as well. I just want to maybe expand on that a little bit more of what is sensory integration? Because I think it leads into biofeedback, I'm assuming pretty quickly. But just like as you work with somebody who may experience dysregulation, anxiety, mental health issues, just how do you position sensory integration to help people regulate their nervous system?
[00:05:23] Speaker B: Very good question. And I think it's so fundamental, Matt, because if you think about it, wherever we move, our whole being is bringing in sensory information.
And we often so much say. My gut feel just tells me. And what does that gut feel mean? It actually means that my sensory systems are accumulating information all the time.
Whether that information is well integrated or whether some systems are more sensitive and others might be a bit more. They need more input to be almost register it. And we call it sort of a low registration. So we've had an amazing sort of OT in the field called Margaret Ayers that really studied kids precisely. Children with autism looked at them, watched them watch their natural progression in movement, what they were seeking, what they were avoiding. And in that way, through intense observation and then creating an sort of optimal environment where they would learn to explore. And in that way the nervous system is calm enough to actually move forward and to explore and learn. Because from birth we are learning.
And whether these systems of ours are well enough integrated might not be. And when trauma comes in, we know there's a moment where in a sense that learning might be interrupted because we then get a fear response, which is a brainstem reflex level, where often the information gets scrambled because a lot of the nuclei in the brain stem are there to almost create the pathway through to different areas in the brain for registration and integration. So we can have. At various points in that pathway we can have a difficulty. So that's where the field of sensory integration has come into. Be able to evaluate effectively, use an effective evaluation system. And then also from there becomes the training to help to reintegrate. And you're right, Matt, like you say, what does the weighted blanket do? It actually helps your proprioceptive feedback system, which is that sense of where I am in space just to help me feel grounded. And when we ground it, it almost creates a space. From here I can move again or from here I can.
Yeah. Gather information because I feel safe. Yeah.
[00:08:06] Speaker A: Beautiful. And if you've never seen an OT at work, it is, you know, really amazing because of the variety. Like we had a, at the school, we had a bouncy chair, which you wouldn't for me would maybe not be necessarily a regulating thing. It'd be kind of more like a fun physical activity. But, but for some youth that the.
That would. Would help them regulate and they could be regulated for an hour or two with this. Other folks, that would be brushing, which I still to this day, if you don't love brushing, you may not be doing it right because it feels, it feels so good to do. But that was regulating for folks. Like I mentioned, the waiting weighted blanket, I think I accidentally like had one on my. I was like, this feels amazing. So I've been sleeping with one ever since because I feel my body in a different way and boy does it help my sleep quality. So it's just a fascinating hands on way to heal. And I love your work. As the audience members know, I got brought to heart rate variability through my work with, with trauma as well. And that did that dysregulation, that disintegration.
And I think a lot of this us in the sensory therapy world has, you know, you all were doing it way before I think we were seriously talking about it. And it's great to see the art, you know, the mental health and the OT world really merge in really cool ways.
[00:09:39] Speaker B: Yeah.
I think we often talk about in OT whether we talk about an arousal system and whether the system, the nervous system is under aroused, it's almost not registered. I can sometimes feel dissociated from my environment because it. The brain is almost not optimized in being switched on. Or it can be so super alert that it's, wow, it's taking in all the information and getting flooded. So you have to understand, and that's what Otis then teach their clients, is to say how unique is your system and what are the strategies that you can use. And that is very individualized.
And you cannot just use one strategy on a lot of people because you have to check out whether brushing is really done effectively and what the client actually needs or not. So I wouldn't say just grab any sensory tool and just apply it.
You need to be regulated in terms of OT watching with you how your nervous system actually responds. So that would be more. I would say a wise decision is in collaboration.
[00:10:53] Speaker A: Yes. You know, absolutely. And, you know, working with youth that would like, you know, which I just got a crash course of, they would actually bang their heads against the wall to help regulate. And it was heartbreaking to see, but for them that was. And obviously we gave them other tools and like, I mean, you know, we're highly motivated to find additional coping skills. But, you know, that that's where I saw OTs of finding out that those replacement behaviors that could be, you know, so I mean, just. And then you saw the growth from, you know, a dysregulated, disintegrated nervous system that banging your head against a concrete wall. In some ways it still baffles me, but would feel good in some ways to much more, you know, way safer, healthier behaviors. I think with trauma, a lot of people can use substances and drugs to help regulate that dysregulated, disintegrated nervous system, obviously, which can become detrimental very quickly for that behavior. So OT is just kind of this brilliant, healthy way to do the integration piece with things. It's an awesome, awesome feel.
[00:12:14] Speaker B: Thank you.
[00:12:15] Speaker A: So I would love to shift because this is where I got really excited looking at your bio with biofeedback as well. So now that we sort of set the foundation for occupational therapy and what you can do in 15, 20 minutes, I would love to kind of learn about what got you interested in biofeedback and how you integrated into your work, you know, as. As an OT or integrated ot, as a biofeedback practitioner. So let's Start out with what, what got you interested in it, and then we'll. We'll go from there.
[00:12:53] Speaker B: Yeah. No, it is a journey. About 20 years ago that I started because in mental health, we were looking at, a lot of adults were sort of diagnosed with adhd.
And you don't necessarily have a sensory room like you would have for the younger kids where you can immediately teach them. So I needed another tool that was going to give me and my client a better window into understanding their arousal system. And that's where biofeedback came in. So we could put a sensor on, say, for instance, the shoulder or the jaw so that they can see how much tension they're holding in their body. Hey. We can put a respiration band on so that we can track effective breathing and retrain that and then combine it with blood volume, pulse, or EKG to get into the domain of heart rate variability, which is such a beautiful tool for arousal regulation. Hey.
And then with that, you can also train effective relaxation. And you can monitor, for instance, peripheral sort of finger temperature because it gives you a good indication of when your client is really relaxing because temperature will increase because as we relax, blood flow can happen more easily. So it's a. A beautiful window that biofeedback gives you as a clinician, not just observing, but giving accurate measurements to be able to help your client understand and for you also as a clinician, to have a different window in. So very excited to learn all of those modalities. And then also added eeg because that is sort of like a little stethoscope that you listen into. How is the brain that firing up this nervous system? Hey.
Yeah. So it's a beautiful tool for helping clients to learn about themselves. But then also it becomes a training domain. So whatever we can measure, we can then retrain so I don't have to stay stuck in a fight flight reflex zone. Once I know, ah, that is how it feels, then I can start understanding how my physiology works and I can start redirecting what the nervous system sort of jumps into and not just be beholden on what the reflex level of the nervous system is.
[00:15:31] Speaker A: Yeah, I love it. So I'm curious, with all these tools in your, your tool belt, what does, what's an assess? How do you like, let's say I'm coming in and seeing you for the first time. Well, what does that, what does that look like for you to sort of craft the mix of OT approaches, you know, HRV, biofeedback, EKGs, all these different tools that you Have.
What's that kind of assessment process look like?
[00:16:02] Speaker B: Yeah, it can be varied, Matt, because it again, depends on the client. If it's a younger child, there will be specific assessments looking at what is developmental sort of achievements looking like. If it's an adult with sort of depression, anxiety or trauma, it will look different because then I will look more at where is the nervous system stuck in. So you have to then make use of various tools and it's where biofeedback is a beautiful measurement because you can go through a stress assessment to show a client. But I find even that can sometimes be too stressful. And I don't want to often compromise the therapeutic situation because I rather want the client to actually realize. But these are tools that we can both engage with. It's not for me to just see in, you know, but it's a discovery sort of journey that we go on together. Often the male and engineer minds come and they want the data. So then I'll give them the dots and we can do 19 channel assessment of EEG and get a good idea and we can compare that to a database for the client's age and gender. So then you've got sort of good data. And you can also then look at heart rate variability, sort of assessment that can give you a good indication of where the starting point is and then track it as you train as well. So, yeah, I think it's data driven, but from an OT perspective, you will always link it back to function. So we will say, okay, so where is the function, the difficulty? Is it because I can't focus?
So how long can I focus before the mind drifts? Yeah. So post stroke, for instance, if I work with a stroke patient, I will look at what are the functional difficulties, whether it is not able to walk effectively or whether it's not able to dress effectively. So it all becomes a functional component.
[00:18:21] Speaker A: I'm curious with your work with trauma and bringing them the mental health pieces in there, because one of the things we've recognized with trauma is that that, that disassociation that, that disintegration that the trauma can cause, you know, also can like we. Our personal narrative or story of ourselves become skewed as well. And I'm curious, from your perspective, do you. Are there individuals who come with a trauma history that you are doing their healing work, or do you usually work with maybe a more traditional talk therapist with that? I'm curious how you approach that with your work because obviously there's the dysregulation of the nervous system I think what I still see in the literature is there is a psychological component to this as well. And obviously if we heal, help heal the nervous system, we're all an integrated system, so we're reintegrating that. But do you see that you can help folks, as the person working with them, get to that post traumatic growth experience, or are you usually working with other folks along the way with that as well?
[00:19:41] Speaker B: I think it depends from client to client. Again, Matt, sometimes clients will come in and they already have got a team, say a psychiatrist and a clinical psychologist, but they want to add bio neurofeedback to help the nervous system so that they can access the trauma processing more effectively. Or sometimes I have clients that come to me first and they don't have a team yet. And so it might be that we start the process, but I will refer because all depending again, what is your scope of practice? So each clinician needs to understand what is their scope of practice and what are they trained in. So if you are trained and trauma informed and you've got other modalities like either somatosensory trauma work that you can bring in, or you can bring in deep brain reorientation work, if you trained in it, yeah, you can combine all of that.
I often start with heart rate variability because people come to me and they dysregulate it and it's scary.
And that is often the window to start with. And then if we see that they actually need more input, I will refer out because I like to work in a team. Sometimes there is need for medication to help the nervous system till it's actually rebuilt itself more effectively over a period of time.
Or sometimes the client then becomes more open and ready to be able to unpack and really look at the trauma and work at that. Sometimes it's not even needed. If you train the right areas of the brain and the right networks of the brain, you can often get that the client, that internal sense of self develops and becomes stronger and they can actually process things already.
Yeah. And sometimes a psychotherapist is needed and we refer, you know.
[00:21:51] Speaker A: Excellent. So the other thing I wanted to ask you about is, you know, you also do work with peak performance as well. And so, so it's one thing to go from somebody who is disregulated, disintegrated because of trauma. I'm curious about, you know, going for working with a population that says, hey, I want to be better at my sport or better at my job or other aspects in life. What, how's that? How do you bring your two, three expertise, four expertise together to work with those folks?
[00:22:31] Speaker B: Because I see it as a continuum, Matt. It's like my athletes might also struggle with anxiety.
[00:22:39] Speaker A: Yeah.
[00:22:41] Speaker B: So then we manage and how that presents within the sport or within, you know, if it. So for me, I always look at optimization. Whether it is optimization in the classroom situation or in relationships or on the sport field, the principles of regulation actually stays the same.
It's the application then of how do I apply it that might be a bit different, you know. And how. How do you help a child to become ready, for instance, for exam time? Very much same principles then getting an athlete ready to compete in a tournament, you know, so same principles. Because it's the same nervous system that will get a sense of dysregulation.
[00:23:31] Speaker A: Hey, you know, very cool. So I want to kind of start to wrap up with a question that is kind of personal to me. But, you know, my heavy work with occupational therapists was about 21, 22 years ago now. And everything I've learned, and I've always been, like, advocating for bringing in ots to every other environment that I've worked in, you know, with children, with. With adults, you know, you need an ot, it's like, well, they're not going to get a job. I'm like, that's not. That's not occupational therapy. And so while I've been an advocate for it, one of the things, you know, that. That I continue to be impressed with occupational therapists is what you all were doing 20 years ago in some ways predicted, where I think psychology and. And the rest of us were going, like, we weren't talking as much about the nervous system. I mean, I know polyvagal theory was out there, but I didn't get it. I mean, I graduated with my master's degree in Psychology in 2000. I didn't get any of that. I didn't get anything really about the brain. We were even talking about trauma back then. So as I, like, got into the OT world, like, not only was I impressed of what they were doing was tangibly working. And, you know, years later, I look back and says, those ots got it. Like they, I. They got it way back when. We weren't even, like, looking at that stuff. So I'm curious, with your experience, you know, in the field, where have you seen. How have you seen OT evolve over time? Now that everybody's talking about the brain, everybody's talking about trauma, everybody's talking about the ventral vagal nerve, you know, all those things.
[00:25:21] Speaker B: Yeah, I think you're quite right. You know, in our, in our primary training we train in neurophysiology alongside the medical fraternity. So you have to have that as a baseline. So all other thinkings and modalities of training will be grounded in that. So neurodevelopment is one of the major things that we are sort of hammered into understanding. So.
Yeah, and I think then it's, it's whether in what domain you work, whether you work with, with children or whether you work with teenagers or adults, it will always play a role and you always will look and go and see where did the impact come, what happened. Whether it's infection, a brain infection, whether it was a traumatic injury of a concussion within a sports field or was it trauma at home over a long period of time, they all have impact. So. And how is it playing out now in this person's life so that they're not optimizing and then you start looking at what tools of development is maybe needed to be trained more. And again, heart rate variability is the strongest bottom up approach. So OTs always talk about bottom up approach because that's what we train and HRV work is one of the strongest ways of regulating brainstem regulation, you know, so, you know, I think it's, it's like you say, it's been there a long time and then I think the, the field of neuroscience is just blown things wider open, more sharing of information.
So I see that various. Otis can apply. How can I say, and bring it into their practice. And that's why I say Otis can be so wide and like you say, what does Otis do? They do everything.
[00:27:29] Speaker A: Yeah.
[00:27:31] Speaker B: They can be community based and work out programs within the community, you know, for.
So it's a diverse sort of domain.
Otis are trained to problem solve. Otis are trained to break down activities, to understand how we do activities as human beings and how important it is from work to social to spiritual to emotional and all of those components.
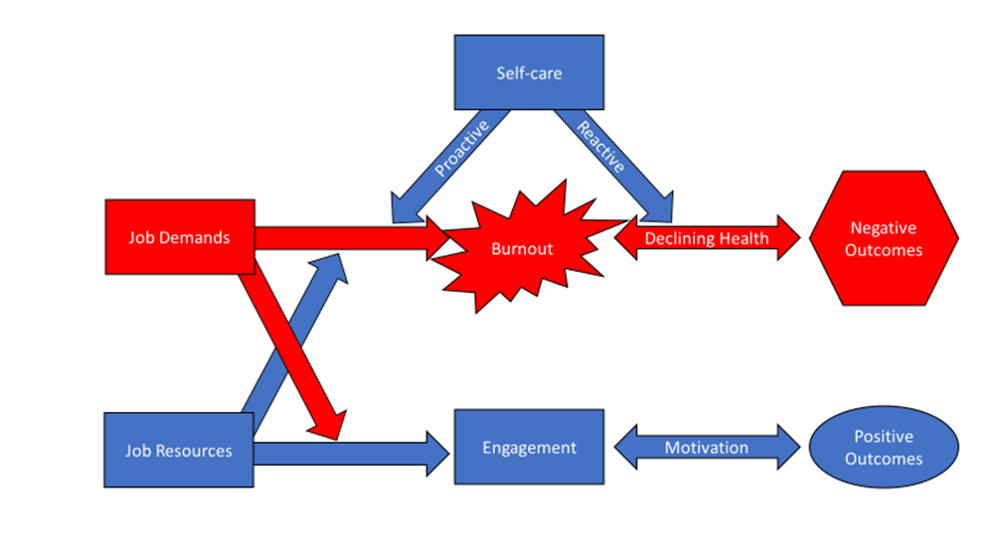
Yeah. Work into a Systems model that OTs often work with you on.
[00:28:08] Speaker A: I, I was just going to leave it there because that's a beautiful way to end. And like I said, I, I was, you know, you, you reached out to me about a question about upcoming training and I, I really appreciate you because the weirdo that you ask a simple question for immediately respond back is, I gotta interview you for this podcast that I do. So I appreciate your willingness to come on and share your work with that and we'll, we'll put information about you, your work web. I got your website up here. Very, very. That's where I, I look. I peeked at that. I was like, oh, I gotta reach out with this. So, hey, I appreciate you, your work in sharing it with our listeners.
[00:28:53] Speaker B: It's a pleasure, Matt. I think the more we network within the world, the better. And I think, luckily, Covid taught us that, that we can network even though we feel at different poles and isolated. So I think thank you for your work that you do. And yeah, let's see how we can connect the world so that we can all grow.
[00:29:15] Speaker A: Absolutely. I would love and will love taking that journey with you. So as always, you can find show notes and other
[email protected] thank you for joining us. And we'll see you next week.